Knowledge Center


From 3 Meetings to 1: Remove Bottlenecks with AI-Enabled eCOA
This webinar, featuring a product demo, will showcase how AI-enabled eCOA is easing those burdens today. Live in numerous studies, this technology already helps top pharma sponsors and CROs consolidate three meetings into just one, achieve 35X faster first-time eCOA creation, and gain back 4–6 weeks to focus on science and patients.


Latest Blogs


What happened at JPM 2026?
Each January, the J.P. Morgan Healthcare Conference sets the tone for the life sciences industry, serving as the year’s most influential gathering of biotech, pharma, investors, and dealmakers.
This year was no different.
Thus, we checked in with our conference attendees, booth visitors, and more to see what they thought were this year’s trend-setting takeaways.

How Agentic AI is transforming life sciences discovery and operations
The numbers are in, and they spell change for life sciences.
That’s because nearly three-quarters (73%) of global pharmaceutical organizations are actively planning, piloting, or deploying agentic AI initiatives.
This widespread means agentic AI is no longer a futuristic concept, but a present-day imperative for staying competitive and delivering life-changing medicines faster.
For those not yet in the know, agentic AI is a sophisticated form of AI designed not just to analyze data, but to act autonomously, plan, reason, and execute complex, multi-step tasks. This goes far beyond traditional automation. Instead, agentic AI is about creating intelligent systems that can drive innovation, accelerate drug development, and optimize operations like never before.
So, which companies are leading the charge, and how exactly are these intelligent agents reshaping the pharma landscape? Let's dive into the specifics.


Playing catch-up: FDA wants “patient’s voice” ePRO in your oncology trial
For years now, the FDA has been making one point crystal clear to sponsors and CROs across our industry; they want the patient voice incorporated whenever possible in oncology trials.
The FDA's initiative is driven by the recognition that a patient's personal experience with a disease and its treatment is a unique and essential measure of a medical product's benefit and risk.
- Rationale: The FDA explicitly states that "patients provide a unique perspective on treatment effectiveness" and "some treatment effects are known only to the patient." Outcomes that truly matter to patients, such as functioning, quality of life, and the burden of side effects, are often best measured directly by the patient.
- Mandate: The Patient-Focused Drug Development (PFDD) effort, codified in part by the 21st Century Cures Act, requires the inclusion of such patient experience data in clinical research.
- Guidance series: To formalize this approach, the FDA has released a series of methodological guidance documents (the PFDD Guidance Series) that outline how stakeholders should collect, submit, and use patient input to inform medical product development.
White papers, Case studies & reports

Medable oncology solutions
Discover how Medable’s AI-powered oncology platform simplifies complex cancer trials by integrating eCOA, ePRO, and eConsent solutions—reducing trial time, improving patient retention, and enhancing data quality for faster, more efficient research.


Driving a high-adherence LTFU trial without an EDC
Learn how Medable is powering a decade-long, global long-term follow-up (LTFU) obesity study, achieving an impressive 97% patient retention rate without using a traditional EDC system all while delivering a compliant, scalable, and cost-efficient solution.


Eliminate clinical trial white space with the right AI strategy
It has become clear that our industry has reachedthe limits of human-only clinical development. As clinical trials have become increasingly complex, the endeavors that people alone can perform are no longer sufficient to generate the momentum needed to address the growing burden of human disease. This has led to longer drug development timelines and significant delays for patients. One large are of lost time is “white space,” definied simply as unproductive time caused by manual, sequential processes and fragmented data systems. Thankfully, a solution lies in agentic AI and its abilities to perform series of tasks.
On-Demand Webinars


Faster Trials, Programmatic Scale: Standardizing a Digital Approach Across Therapeutic Areas
Explore how AI and standardization are transforming clinical trial efficiency across multiple therapeutic areas in this expert-led webinar.
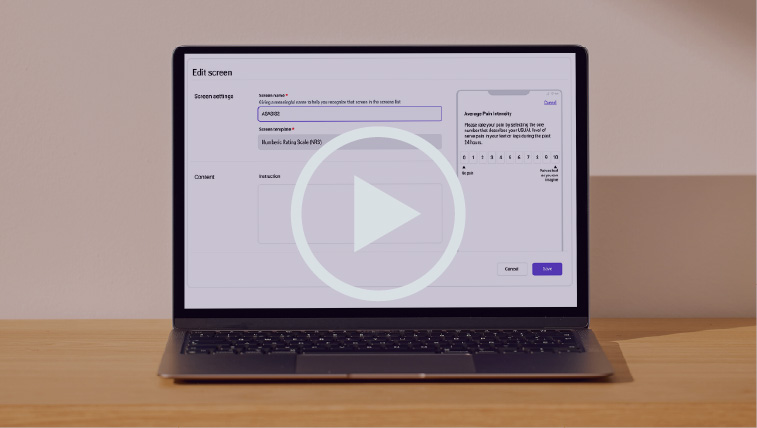

From complexity to clarity: Automate eCOA configuration with AI
Clinical trials are more complex than ever, but building and launching global studies doesn’t have to be. Watch alive demo of our AI-powered eCOA platform to learn more.


Not just a tool: How AI agents become trial teammates
Explore how agentic AI is transforming clinical trials by automating routine tasks and boosting team efficiency with real-world, low-risk use cases.
Scientific Research

Assessing the financial value of decentralized clinical trials
Deployment of remote and virtual clinical trial methods and technologies, referred to collectively as decentralized clinical trials (DCTs), represents a profound shift in clinical trial practice. To our knowledge, a comprehensive assessment of the financial net benefits of DCTs has not been conducted

Development of a mobile health app (TOGETHERCare) to reduce cancer care partner burden: Product design study
Research looking at mobile apps and how they may provide a meaningful access point for all stakeholders for symptom management.
Guides


Vertical vs. horizontal: Why your Agentic AI should be built by clinical experts in life sciences
By now, most people are familiar with ChatGPT and other general-purpose AI tools such as Perplexity. These horizontal AI systems have become commonplace, assisting users with tasks like composing emails, summarizing information, or generating creative ideas. Their adaptability across a wide range of domains demonstrates the power of general intelligence and transfer learning.
However, in the high-stakes and highly regulated context of life sciences, it is important to ask whether such tools are suitable for clinical use. In this setting, a vertical agentic AI approach—purpose-built for specific domains—provides the precision, reliability, and compliance necessary for success. While both horizontal and vertical agentic AI play essential roles in the broader evolution of intelligent systems, it is the vertical approach that ensures the rigor and accountability demanded by life sciences applications.


Building blocks: The ultimate guide to AI in clinical trials
Explore how artificial intelligence (AI) is fundamentally transforming every facet of clinical trials, from initial protocol design and patient recruitment to data management and regulatory approval. This comprehensive guide provides an authoritative, in-depth look at AI's role in accelerating drug development and improving patient outcomes, with special focus on emerging agentic AI technologies.