
Related articles


eCOA standards and KPIs to include in your next RFI
According to Gartner, a request for information, or a request for proposal, is defined as “both the process and documentation used in soliciting bids for potential business or IT solutions required by an enterprise or government agency. The RFI document typically outlines a statement of requirements (SOR) to be met by prospective respondents wishing to make a bid to deliver the required solutions. It might cover products and/or services to meet the given requirements.”
Yet, for anyone entering into a long-term business agreement, a well-written RFI can do so much more than just assess and collect vendor capabilities.
For the last decade, Medable has been transforming the capabilities of organizations across clinical research using the latest in new technologies. In this time, we’ve learned the best RFIs are able to define what success looks like, create alignment on measurable outcomes, and establish accountability on roles and responsibilities well before a contract is ever signed. When done correctly, it becomes a decision-making framework that offers clear vision to both organizations.
Recently, Medable received two RFIs around eCOA from top pharmaceutical organizations. They stood out to us because they were structured around performance, not promises, a distinction that makes all the difference.
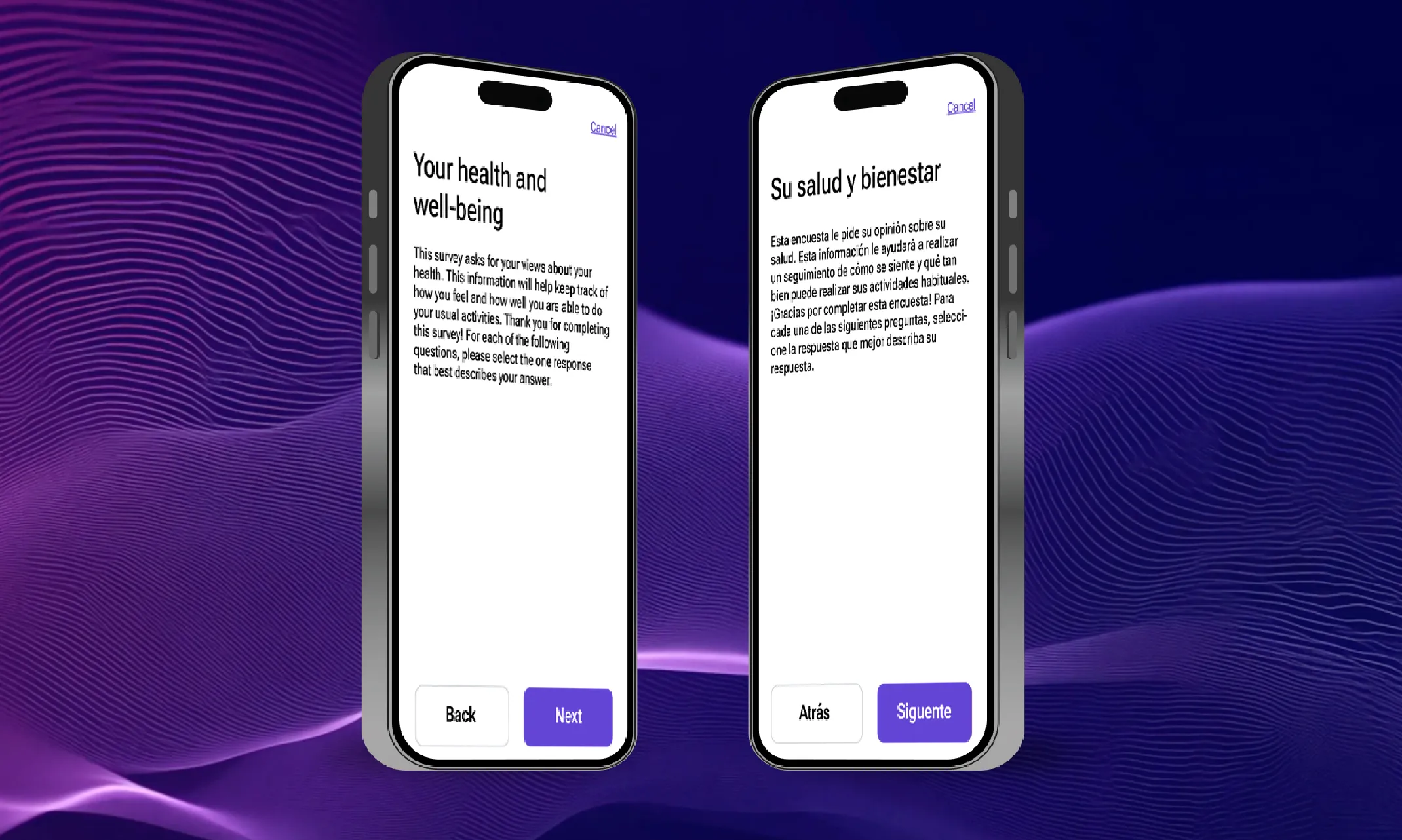

From bottlenecks to breakthroughs: How AI is transforming translation timelines
According to ClinicalTrials.gov, there are 3,046 multi-country trials being conducted this year. While many trials remain localized within a single country, there has been a definitive movement towards conducting trials in multiple countries, especially for larger, later-stage trials. This is driven by the positives that multi-country trials offer, like faster patient recruitment, lower costs in some regions, and the need for diverse patient populations.. However, behind the scenes, a critical bottleneck has been slowing many trials down. This bottleneck is the translation process that’s required to make trials work across multiple languages, locales, and regulatory bodies/organizations.


The Top 5 myths about eCOA in 2025
With MarketsandMarkets projecting the global electronic Clinical Outcome Assessments (eCOA) solutions market to grow at compound annual growth rate (CAGR) of 16.1% each year until 2030, it’s clear the eCOA has made its impact within the clinical research landscape.
Yet despite growing adoption, electronic Clinical Outcome Assessments (eCOA) are still surrounded by misconceptions that hinder their full potential. From concerns about patient usability to assumptions about cost and implementation timelines, these myths can create hesitation among sponsors and research teams alike.
Thus, we’re here to cut through the noise and set the record straight with a summary of a recent webinar featuring speakers from Transcelerate and Medable.




