For years now, the FDA has been making one point crystal clear to sponsors and CROs across our industry; they want the patient voice incorporated whenever possible in oncology trials.
The FDA's initiative is driven by the recognition that a patient's personal experience with a disease and its treatment is a unique and essential measure of a medical product's benefit and risk.
- Rationale: The FDA explicitly states that "patients provide a unique perspective on treatment effectiveness" and "some treatment effects are known only to the patient." Outcomes that truly matter to patients, such as functioning, quality of life, and the burden of side effects, are often best measured directly by the patient.
- Mandate: The Patient-Focused Drug Development (PFDD) effort, codified in part by the 21st Century Cures Act, requires the inclusion of such patient experience data in clinical research.
- Guidance series: To formalize this approach, the FDA has released a series of methodological guidance documents (the PFDD Guidance Series) that outline how stakeholders should collect, submit, and use patient input to inform medical product development.
The mechanism: Patient-reported outcomes (PROs) and ePRO
The primary method the FDA encourages sponsors to use for collecting the patient's voice is through Clinical Outcome Assessments (COAs), with Patient-Reported Outcomes (PROs) being the most relevant type for direct patient input.
- PRO (Patient-Reported Outcome)
- A measurement based on a report that comes directly from the patient about their health status without interpretation by a clinician or anyone else.
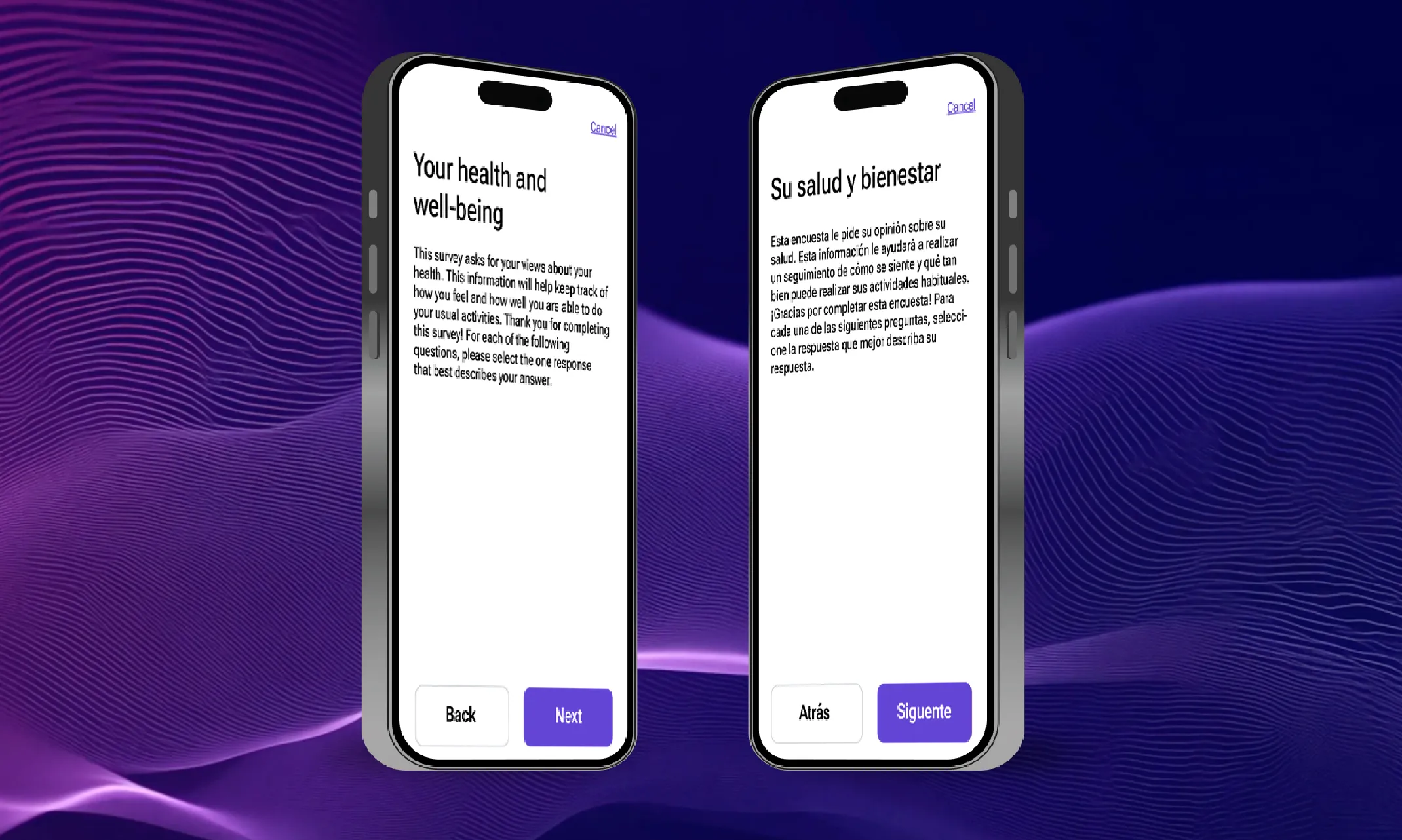
- ePRO (Electronic PRO)
- The delivery and data capture of a PRO instrument using electronic systems (e.g., tablets, smartphones, interactive voice response (IVR) systems).
Unfortunately, between 2010 and 2020, only 9 out of 108 FDA-approved oncology drugs, a mere 8.3%, included electronic patient-reported outcomes (ePROs) in their labeling.
Clearly, ePRO adoption is lagging in oncology trials. This comes despite recent guidance from the FDA (in 2021 and 2024) explaining how sponsors can use these technologies to ease trials for themselves and their patients.
FDA's view on ePRO
The FDA strongly encourages the use of electronic modalities (ePRO) over traditional paper-based methods for several critical reasons:
Patient burden
- ePRO benefit: ePRO allows for advanced techniques like Computer Adaptive Testing (CAT), which efficiently uses fewer questions to generate a precise score, thereby reducing the patient's questionnaire burden. It also enables sponsors and CROs to use digital methods to overcome challenges, such as auto-narrated ePROs that offer a workaround for visually impaired patients.
FDA guidance/preference: The FDA emphasizes the need to minimize patient fatigue and burden to "maximize the quality and completeness of information collected."Data integrity
- ePRO benefit: Electronic systems automatically time-stamp responses and prevent the secondary data entry errors that are common with paper forms.
- FDA guidance/preference: The FDA prefers the electronic capture of clinical trial source data, citing it as essential for improving data quality and integrity.
Compliance
- ePRO benefit: ePRO systems can provide reminders and alerts, which helps patients adhere to the assessment schedule, creating more complete data. This is in stark contrast to paper, which often fails to meet the basic ALCO requirements of a reported outcome.
- FDA guidance/preference: Real-time data access allows sponsors to monitor compliance and proactively encourage patient reporting, a capability impossible with traditional paper diaries.
Data accuracy
- ePRO benefit: ePRO allows for real-time, at-the-moment data capture for episodic or daily symptoms (e.g., pain, nausea, urinary urgency). This prevents the recall bias that occurs when patients fill out a paper diary just before a clinic visit.
- FDA guidance/preference: The agency recommends delivering Clinical Outcome Assessments (COAs) in a way that is most convenient to patients, strongly suggesting the use of electronic methods for conditions that require frequent, event-based reporting.
Sponsor requirements for ePRO implementation
In its guidance on the use of PRO measures, the FDA provides specific, detailed recommendations to sponsors to ensure the validity, integrity, and security of ePRO data:
Data and system integrity
- 21 CFR Part 11 compliance: ePRO systems must be fully compliant with 21 CFR Part 11, including maintaining a clear, immutable audit trail that captures any changes made to the data.
- Investigator accountability: The clinical investigator (the site doctor) remains primarily responsible for the subject's data. PRO data should not be modified without the investigator's involvement.
- Data control: Exclusive control of source documents by the sponsor is expressly discouraged.
- Database security: Sponsors must ensure there is robust database backup to mitigate the risk of data loss or corruption during the trial.
Trial design and blinding
- Timely access to safety data: Systems must ensure direct transmission of important safety information, for example, patient-reported symptomatic adverse events, to the clinical investigator in a timely manner for patient care and safety monitoring.
- Unblinding prevention: Sponsors must take precautions to prevent premature or unplanned access to unblinded data. If the treatment has obvious effects that could unintentionally unblind a patient (affecting their PRO responses), the sponsor is encouraged to use PRO administration techniques to minimize bias.
- COA validation: The PRO instrument itself must be rigorously validated. This process should ideally be complete before the start of a pivotal Phase 3 trial to ensure it is "fit-for-purpose" and accurately measures the concepts that are meaningful to the patient.
Why ePRO is Ideal for oncology
- Capturing nuanced side effects: Newer targeted cancer therapies often produce chronic, low-grade side effects that are easily missed during intermittent clinic visits but significantly impact a patient’s life. ePRO provides a direct, unfiltered, and real-time capture of this symptom burden.
- Reducing trial fatigue: Oncology trials are often lengthy and involve significant travel and procedural burdens. By allowing remote symptom reporting, ePRO reduces the overall fatigue associated with trial participation, which, in turn, enhances patient compliance and data completeness.
- Informing treatment decisions: Data from ePRO provides essential insights into:
- How symptoms impact a patient's daily life.
- Their functional status during treatment.
- Their quality of life considerations.
- Regulatory endorsement and standardization:
- The FDA has created initiatives like "Project Patient Voice" to consistently showcase patient-reported symptom data from cancer trials of approved products. This data (such as the worsening of nausea reported in the Aura3 trial example) provides a clear picture of the full risk/benefit profile of a drug.
- The use of standardized systems, such as the Patient-Reported Outcomes version of the Common Terminology Criteria for Adverse Events (PRO-CTCAE), in an electronic format (ePRO) ensures data consistency across studies. This creates a more robust dataset that can influence not only regulatory decisions but also clinical practice guidelines for physicians.
A real-life example: Aura3 data
For a real-life example, consider the FDA’s “Project Patient Voice,” an initiative that aims to “show patient-reported symptom data consistently from select cancer clinical trials of approved products.”
Their Aura3 data show the changes in quality of life that some participants experienced as they progressed through the trial. According to the FDA, “before starting treatment, 25% of patients who received the trial drug reported having nausea (ranging from rarely to almost constantly).
After beginning treatment, 41% of patients who received the trial drug reported their nausea had worsened (increased by at least 1 point on a 0 – 4 scale) at any time while on treatment. After starting treatment, 6% of patients who received the trial drug reported their nausea had worsened to either occurring frequently or almost constantly at any time while on treatment.”
As the data shows, we can see that participants experience a myriad of effects during a trial that the industry is increasingly expected to capture and report.
By integrating ePRO, sponsors can fundamentally change how cancer therapies are developed, ensuring the patient's voice is central to the process and leading to treatments that focus not just on extending life, but improving its quality.
Don’t get left behind: Make the patient voice central to your next trial
The FDA has clearly signaled the path forward: integrating the patient's voice through ePRO is no longer a luxury; it's a regulatory expectation, especially in complex oncology trials where quality of life data is paramount.
The low historical adoption rate of ePRO in oncology labeling shows that the industry is playing catch-up, missing opportunities to gather the crucial, real-time data the FDA demands.
To stay ahead of the curve and fully meet the requirements of the PFDD initiative, your trials need a flexible, compliant, and patient-centric ePRO solution.
Explore Medable's unified, validated ePRO platform and see how we're making it easy to capture the patient's voice across the globe.