Knowledge Center


Innovation Evidence : A Tufts CSDD workshop
In the five years since the pandemic, decentralized trial elements have solidified their status in medical product development.
Trials with decentralized elements have moved past the “pilot” phase. The question is no longer whether we can operationalize decentralized trial components, it's whether we’re doing it thoughtfully at the pace patients deserve. Our industry is ready to optimize the elements for the trial based on available evidence.
That’s exactly why Medable, in collaboration with and facilitated by the Tufts Center for the Study of Drug Development (Tufts CSDD), has launched the Innovation Evidence Workshop series.
Last November, the inaugural, invitation-only workshop brought leaders from 20 pharmaceutical, biotech, and CRO organizations together in Boston, with representation from the U.S. Food and Drug Administration, Harvard MRCT Center, Tufts CSDD, and Medable.
Latest Blogs


Compounding interest: Why “good enough” data is good enough for agentic AI
Let’s ask a trick question.
Do you think your organization’s data is ready for AI, or AI Agents?
Most sponsors and CROs instinctively answer “not yet.” What this really means is that they don’t believe their data isn’t fully centralized, dictionaries aren’t perfectly aligned, and too many systems still operate in parallel. The result is that AI gets parked on the roadmap, waiting for a future state where everything is clean, standardized, and coordinated.
Here’s the twist; waiting for that moment is very thing holding organizations back.
When it comes to implementing agentic AI, the bigger risk right now isn’t imperfect data. Instead, it’s waiting for perfection before acting.


eCOA standards and KPIs to include in your next RFI
According to Gartner, a request for information, or a request for proposal, is defined as “both the process and documentation used in soliciting bids for potential business or IT solutions required by an enterprise or government agency. The RFI document typically outlines a statement of requirements (SOR) to be met by prospective respondents wishing to make a bid to deliver the required solutions. It might cover products and/or services to meet the given requirements.”
Yet, for anyone entering into a long-term business agreement, a well-written RFI can do so much more than just assess and collect vendor capabilities.
For the last decade, Medable has been transforming the capabilities of organizations across clinical research using the latest in new technologies. In this time, we’ve learned the best RFIs are able to define what success looks like, create alignment on measurable outcomes, and establish accountability on roles and responsibilities well before a contract is ever signed. When done correctly, it becomes a decision-making framework that offers clear vision to both organizations.
Recently, Medable received two RFIs around eCOA from top pharmaceutical organizations. They stood out to us because they were structured around performance, not promises, a distinction that makes all the difference.


Paper COAs in 2026? It’s not “cheaper,” it’s riskier
eCOA’s time has come. The market is currently estimated to be worth $2.3 billion, with projections showing it reaching nearly $5 billion by 2030. Despite this, paper still plays a prominent role for some clinical trials today.
At first glance, paper may seem simple and familiar, even economical. However, in today’s regulatory and operational environment, paper COAs are not a risk averse choice when held to the standards of what sponsors, CROs, and regulators are looking for trial data to prove.
White papers, Case studies & reports
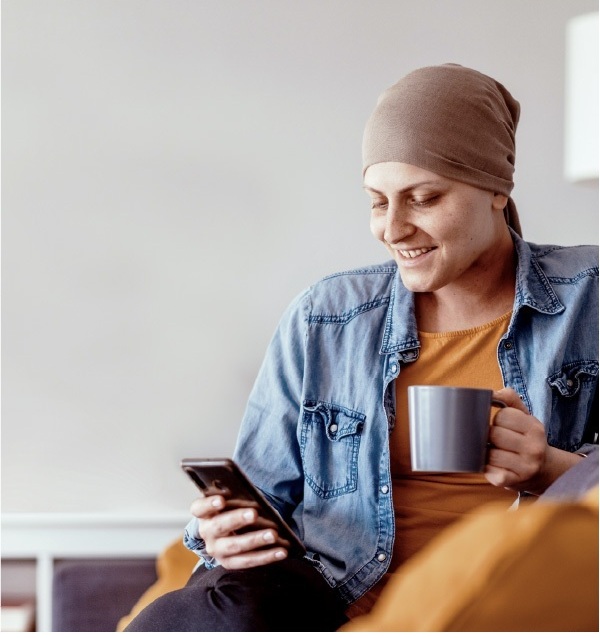

Medable oncology solutions
Discover how Medable’s AI-powered oncology platform simplifies complex cancer trials by integrating eCOA, ePRO, and eConsent solutions—reducing trial time, improving patient retention, and enhancing data quality for faster, more efficient research.


Driving a high-adherence LTFU trial without an EDC
Learn how Medable is powering a decade-long, global long-term follow-up (LTFU) obesity study, achieving an impressive 97% patient retention rate without using a traditional EDC system all while delivering a compliant, scalable, and cost-efficient solution.


Eliminate clinical trial white space with the right AI strategy
It has become clear that our industry has reachedthe limits of human-only clinical development. As clinical trials have become increasingly complex, the endeavors that people alone can perform are no longer sufficient to generate the momentum needed to address the growing burden of human disease. This has led to longer drug development timelines and significant delays for patients. One large are of lost time is “white space,” definied simply as unproductive time caused by manual, sequential processes and fragmented data systems. Thankfully, a solution lies in agentic AI and its abilities to perform series of tasks.
On-Demand Webinars


Faster Trials, Programmatic Scale: Standardizing a Digital Approach Across Therapeutic Areas
Explore how AI and standardization are transforming clinical trial efficiency across multiple therapeutic areas in this expert-led webinar.
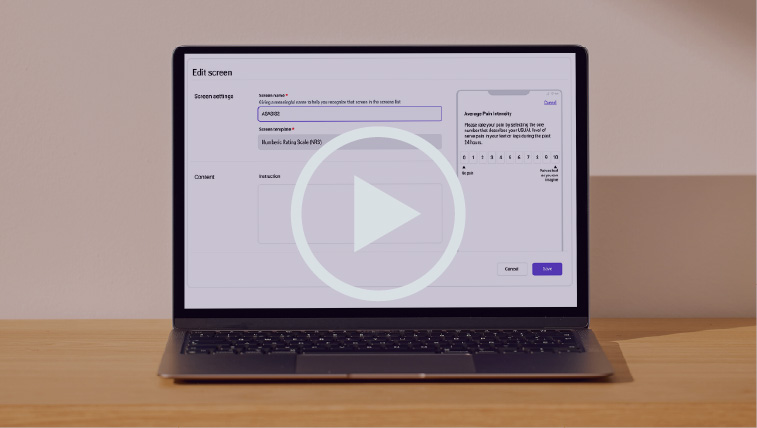

From complexity to clarity: Automate eCOA configuration with AI
Clinical trials are more complex than ever, but building and launching global studies doesn’t have to be. Watch alive demo of our AI-powered eCOA platform to learn more.


Not just a tool: How AI agents become trial teammates
Explore how agentic AI is transforming clinical trials by automating routine tasks and boosting team efficiency with real-world, low-risk use cases.
Scientific Research

Assessing the financial value of decentralized clinical trials
Deployment of remote and virtual clinical trial methods and technologies, referred to collectively as decentralized clinical trials (DCTs), represents a profound shift in clinical trial practice. To our knowledge, a comprehensive assessment of the financial net benefits of DCTs has not been conducted

Development of a mobile health app (TOGETHERCare) to reduce cancer care partner burden: Product design study
Research looking at mobile apps and how they may provide a meaningful access point for all stakeholders for symptom management.
Guides

How to successfully transition from paper COAs to eCOA
Electronic clinical outcome assessment (eCOA) systems have reshaped how patient-reported outcome measures are collected and managed in clinical trials. Clinical operations leaders are under more pressure than ever to ensure that the migration from legacy paper instruments to digital platforms not only improves trial efficiency but also preserves data integrity, supports regulatory acceptance, and enhances participant experience.
The transition from paper to electronic capture represents a paradigm shift toward more efficient, accessible, and reliable data collection. Done well, eCOA strengthens evidence generation while reducing burden for participants and sites alike. Done poorly, it risks measurement bias, loss of comparability, and regulatory challenges.
In this article, clinical operations leaders will find evidence-based best practices for migrating and implementing patient-reported measures as part of eCOA strategies. These recommendations are rooted in published industry guidance and emerging scientific consensus, and they reflect the evolving landscape of digital assessment technologies.

Common eCOA implementation pitfalls and how to avoid them
The global eCOA (electronic clinical outcome assessment) solutions market was valued at over two billion dollars in 2025, and is projected to expand rapidly over the coming decade, driven by increased clinical trial activity, digital transformation efforts, and the integration of mobile, cloud, and AI-enabled tools for outcome measurement.
This growth reflects not just broader industry digitization, but an evolving expectation: that outcome data should be accurate, audit-ready through validated systems and controlled operational processes, and capable of supporting decentralized workflows.As more sponsors and CROs incorporate eCOA into their trial strategies and regulators continue to emphasize electronic data integrity the stakes of successful implementation have never been higher.
Yet with greater adoption comes greater complexity: pitfalls around site burden, mid-study amendments, device logistics, and training gaps can undermine even the most advanced platforms if not thoughtfully addressed.
The good news? These common challenges can be anticipated and managed with practical, operationally aligned planning turning eCOA from a source of friction into a strategic advantage for trial success.


Vertical vs. horizontal: Why your Agentic AI should be built by clinical experts in life sciences
By now, most people are familiar with ChatGPT and other general-purpose AI tools such as Perplexity. These horizontal AI systems have become commonplace, assisting users with tasks like composing emails, summarizing information, or generating creative ideas. Their adaptability across a wide range of domains demonstrates the power of general intelligence and transfer learning.
However, in the high-stakes and highly regulated context of life sciences, it is important to ask whether such tools are suitable for clinical use. In this setting, a vertical agentic AI approach—purpose-built for specific domains—provides the precision, reliability, and compliance necessary for success. While both horizontal and vertical agentic AI play essential roles in the broader evolution of intelligent systems, it is the vertical approach that ensures the rigor and accountability demanded by life sciences applications.



