Related articles


Driving a high-adherence LTFU trial without an EDC
Learn how Medable is powering a decade-long, global long-term follow-up (LTFU) obesity study, achieving an impressive 97% patient retention rate without using a traditional EDC system all while delivering a compliant, scalable, and cost-efficient solution.


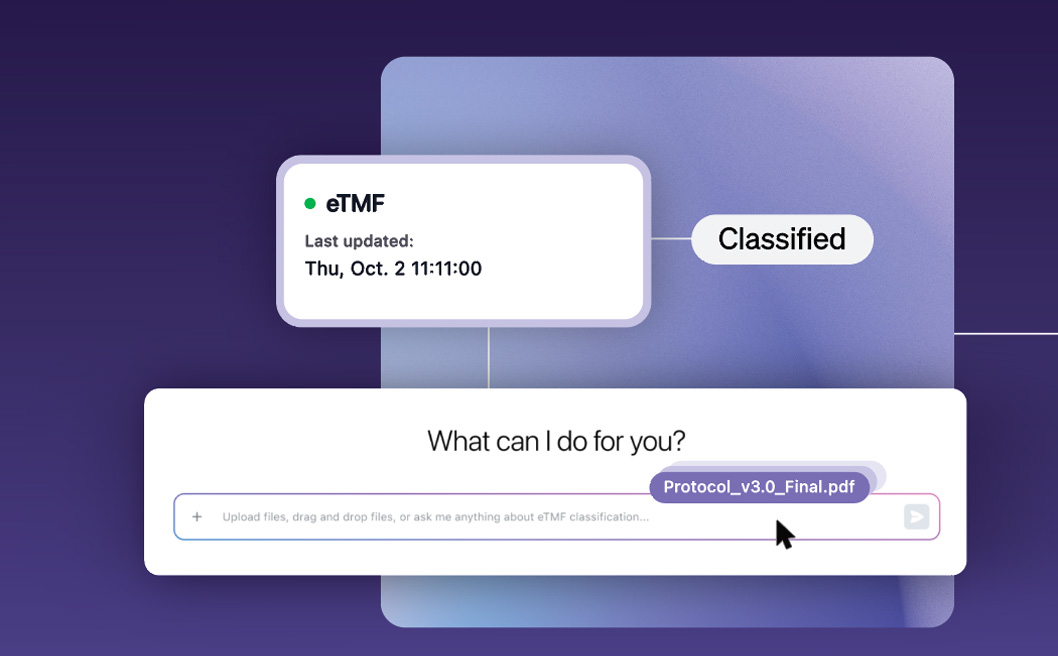
Eliminate clinical trial white space with the right AI strategy
It has become clear that our industry has reachedthe limits of human-only clinical development. As clinical trials have become increasingly complex, the endeavors that people alone can perform are no longer sufficient to generate the momentum needed to address the growing burden of human disease. This has led to longer drug development timelines and significant delays for patients. One large are of lost time is “white space,” definied simply as unproductive time caused by manual, sequential processes and fragmented data systems. Thankfully, a solution lies in agentic AI and its abilities to perform series of tasks.

Six steps to help you choose the right clinical trial partner
“This year, we’ve decided to stick to paper. We know what we’re getting and we’ve always done it this way.”
That was the unwavering response from a clinical operations lead at a pioneering biotech when asked why they still relied on paper diaries for patient-reported outcomes.
Despite the growing complexity of global trials, the promise of real-time data, and the surge of digital capabilities available today, some organizations have held tight to a method of clinical trial conduct that’s increasingly as outclassed as it is outdated.
It’s well known that individuals and organizations believe that change can be daunting, stressful, and difficult, especially when the old way is familiar and entrenched. However, much like anything else, having a partner who can help guide you through the process is massively important. But, how do you find the right partner for your trials?
Before locking in a vendor, organizations must engage in a deliberate process to assess their needs, align stakeholders, and set the foundation for long-term success. This blog explores the critical steps sponsors should take before selecting a digital partner, using insights and frameworks drawn from Medable’s therapeutic area standards and industry best practices.